If we don’t want to see a repeat of last fall’s devastating respiratory illness season that claimed the lives of six B.C. children, now’s the time to do something about it.
That’s the message Protect Our Province BC sent out at a briefing this afternoon (Wednesday, June 28).
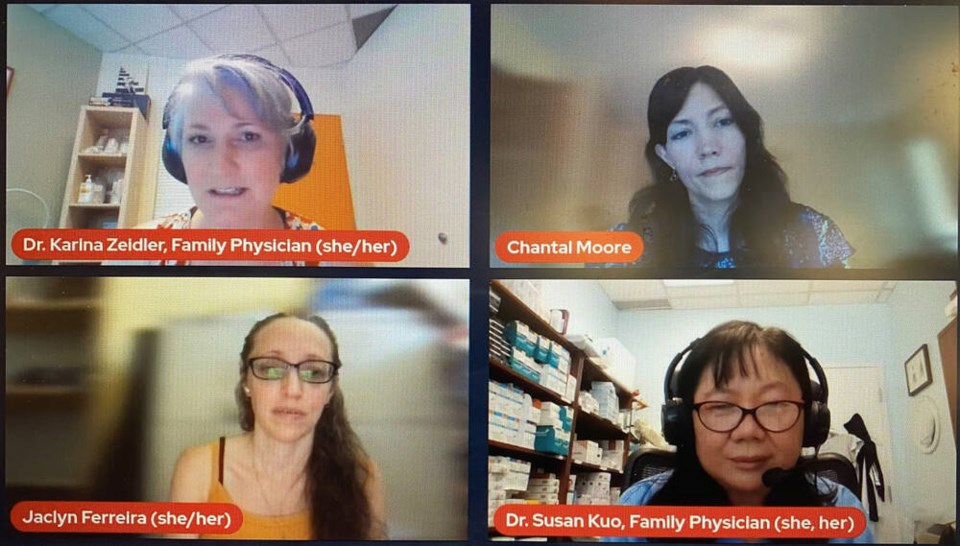
Dr. Karina Zeidler noted Protect Our Province BC — a grassroots advocacy group made up of doctors, nurses, healthy scientists, health policy specialists and community advocates — started its work in 2021, advocating for better COVID-19 protections for students and school staff.
“Here we are two years later doing the same thing, advocating for many of the same things,” she said.
The briefing included speakers Jaclyn Ferreira, a researcher, parent and disability inclusion advocate; Dr. Susan Kuo, a family physician from Richmond and a clinical associate professor in UBC’s Faculty of Medicine; and Chantal Moore, a parent and science communicator.
Ferreira said the 2022-23 school year, which is just wrapping up, was the worst year for the health of children since the beginning of the COVID-19 pandemic. Cases in point: last fall’s “tripledemic” of flu, COVID-19 and RSV, the “overstretched and overflowing” pediatric emergency rooms, the shortage of children’s cold and flu medications, and the high rates of teacher and student absenteeism in schools.
Six B.C. children died of flu in the fall of 2022.
Respiratory illness warning signs starting in Southern Hemisphere
Ferreira said that all happened despite the warning signs coming from the Southern Hemisphere after unprecedented rates of pediatric illnesses and hospitalizations during their winter (our summer) in 2022.
“There was no reason to presume that the same fate wouldn’t face B.C.’s children in our then upcoming winter season, but we ignored the signals,” she said. “Flash forward to the Southern Hemisphere right now in their winter of 2023, and we are seeing similar patterns emerging.”
The news from Australia and South America right now shows high rates of COVID, an early flu season and a significant growth in RSV hospitalizations, Ferreira pointed out.
Right now, she said, is when B.C. needs to act to make sure it doesn’t follow in those footsteps again.
“COVID and other viruses rely on human behaviour, and ignoring what we can see happening in other countries while continuing to act like the pandemic is over will bring on the next wave,” she said. “That is a mathematical fact.”
'I've never seen so many sick people': Richmond doctor
Kuo said last year was the worst season she’s ever seen.
“In the 30 years I’ve been a practising family doctor, I’ve never seen so many sick people,” she said.
She cited a recent study in JAMA (Journal of the American Medical Association) that showed 70 per cent of COVID-19 infections were from children bringing COVID home from schools and daycares to their parents, siblings and grandparents — a pattern she saw in her own practice, where families were “continuously sick” from the cycle.
Plus, she added, B.C. family doctors’ hands were tied by a lack of testing and a lack of medications.
“I’m a family doctor in the 21st century, but last fall I might as well be back in the 19th century because, with no testing and no medications available to me, all I could offer my patients was to hold their hands,” she said. “It was a nightmare. I really hope we don’t have to go through this again.”
Kuo warned that COVID-19 in children is not “mild.”
“It can affect every system in the body and causes diseases such as diabetes and depression. It can damage the immune system, making people more susceptible to infection. This explains the increased cases of strep throat, pneumonia and fungal infections we’re seeing increasing in healthy children,” she said.
Plus, she said, there’s the estimated 10 to 15 per cent of children who don’t get better after their COVID-19 infection and who suffer the effects of long COVID — and the unknowns around how far-reaching the impacts of the COVID-19 virus will be on those infected now.
So what can be done to stem the tide heading into the fall of 2023?
COVID protection requires collective action
First and foremost, Moore said, we need a mindset shift.
“Public health has really set the individual responsibility, ‘you do you’ narrative,” she said. “That narrative does not work. We have to act as a collective. We can’t just think of ourselves, our individual risks, when we make decisions on whether or not to wear a mask. We should really think about the most vulnerable people among us: the elderly, children with chronic diseases and illnesses.”
Moore outlined a version of the “Swiss cheese” philosophy of COVID-19 protection, noting four layers are part of ultimately stopping viral transmission in schools: families, educators, school administrators, and government leaders.
“Our leaders have really sent the message that it’s inevitable you’re going to get COVID, everyone has COVID, this is going to be here forever,” she said. “And we really have to push back on that narrative and really challenge it because it’s not a very hopeful message, and the reality is there are concrete things we can do that are proven to reduce our infection risk and prevent us from spreading the virus to our loved ones.”
Zeidler said there’s much that can be done to help mitigate against the coming respiratory illness season.
“At this point, I think it’s quite clear that we can’t rely on government and public health to bring in protections,” she said. “We’re going to keep putting pressure on them, but that pressure really needs to come from the bottom up.”
Moore outlined a detailed list of steps that can be taken at each level to help stop COVID-19 in its tracks. Some highlights:
What can families do about COVID? Ideas for parents, guardians and students
- Get vaccinated and boosted.
- Mask up in school this September.
- Have a safe plan for lunch (eat outside or in an alternate space, for example).
- Stay home if you’re sick.
- Use rapid antigen tests (RATs) — stock up on them while they’re still available.
- Report known COVID cases to the B.C. School COVID Tracker.
What can teachers do about COVID? Ideas for education workers
- Be a role model: Mask to help students, especially vulnerable students, feel comfortable about masking.
- Understand aerosol spread and educate students about it.
- Space out desks where possible.
- Open windows.
- Turn on HEPA filtration units where possible.
- Advocate to unions and administration for COVID safety protocols.
What can school administrators do about COVID? Ideas for schools
- Understand aerosol spread and educate students and staff about it.
- Wear a mask to be a role model; encourage or require masks in your own school setting.
- Educate students and teachers about the dangers of COVID.
- Use HEPA air filtration and/or do-it-yourself boxes (Corsi-Rosenthal).
What can the provincial government do about COVID? Ideas for B.C. leaders
- Name it: “Be brave: say the word ‘airborne,’” Moore said.
- Educate the public on the reality and risks of long COVID and the risks of repeat infections.
- Mandate masks in the fall respiratory season.
- Conduct a timely, family-friendly vaccine rollout for influenza and COVID-19; make vaccinations available in times and places that are accessible to parents (such as at schools).
- Require clean air in B.C. classrooms — legislate indoor air quality to the latest ASHRAE Section 241 standards around mitigation of airborne infection.
More information and a video of the full briefing can be found at the Protect Our Province BC website.
Follow Julie MacLellan on Twitter @juliemaclellan.
Email Julie, [email protected]